
Understanding the Alarming Rise of Cancer Among Young Adults
In high-income countries like Britain, Denmark, and the US, cancer rates among people under 50 are on the rise. This is a notable shift since cancer has traditionally been associated with old age. The surge in younger cancer patients is concerning, especially as these cases tend to be more aggressive and go undiagnosed for longer periods due to the lack of routine screening.
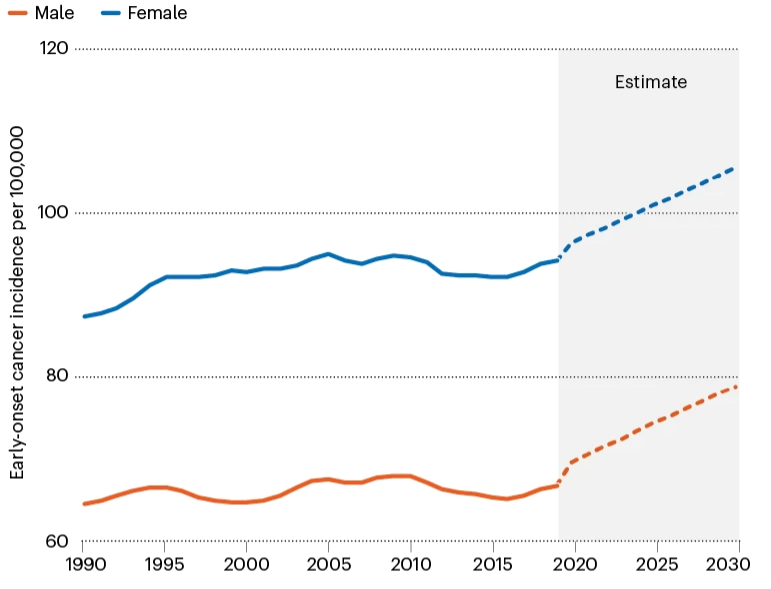
Data from the G20 countries reveals a 22% increase in cancer rates among 25-29-year-olds between 1990 and 2019, with the highest-ever levels seen in the 30-34 age group. This trend is projected to continue, suggesting a concerning “birth cohort effect,” where each successive generation faces a higher cancer risk due to early-life exposures to diet, lifestyle, weight, and environmental factors.
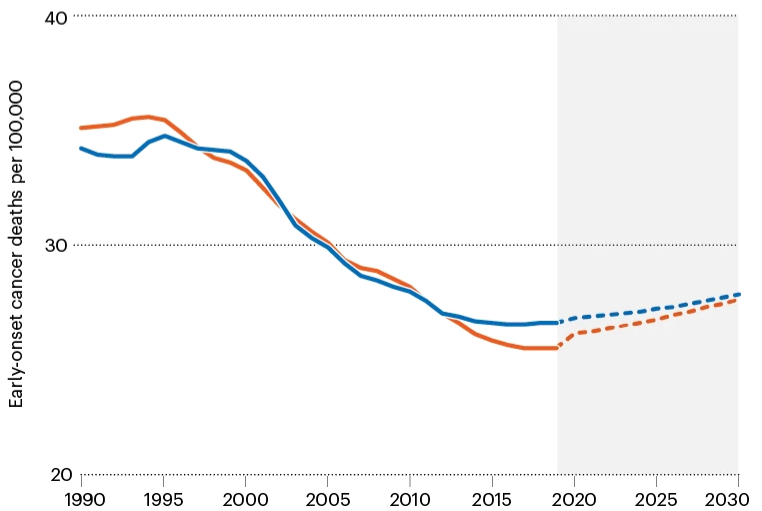
The rise in early-onset cancers is particularly evident in types affecting the digestive system, such as breast, colon, oesophagus, kidney, liver, and pancreas cancer. Colorectal cancer, for instance, surged by 70% among individuals aged 15-39 in G20 countries over the same period. Understanding the specific organs and tissues affected by these cancers can provide insights into the environmental factors contributing to their increase.
Cancer risk factors, including smoking, alcohol consumption, obesity, physical inactivity, and poor diet, are consistent across various cancer types. While the exact role of diet in the rise of cancer among young individuals is not conclusive, experts like Ogino emphasize its significance. Diet’s impact on the microbiome, the community of microbes in the gut crucial for digestion and immune function, is of particular interest in understanding early-onset cancer.

The prevalence of ultra-processed foods, high in saturated fat and sugar, has disrupted the balance of the microbiome, potentially contributing to cancer risk. These foods, though affordable and convenient, pose significant health risks, especially for children. However, their consumption has surged, driven by factors like affordability and appeal.

Alcohol, another major carcinogen, exacerbates the issue, further raising cancer risks. The escalating cost of healthier options like fruits, vegetables, and lean proteins has made ultra-processed foods the primary choice for many families. To address this, policies are needed to make nutritious options more accessible, especially for low-income households.
Tackling the rising cancer incidence among young people requires decisive action, including promoting affordable, healthier food choices and ensuring adequate incomes to afford them. Investing in prevention is paramount for reducing healthcare costs and fostering a productive workforce. Delaying action risks exacerbating the already alarming trend of early-onset cancers linked to poor dietary habits.
Emphasize Diet as a Key Factor

A considerable portion of my work involves dispelling dietary misconceptions surrounding cancer. Questions often arise about sugar’s role in fueling cancer, the dangers of meat consumption, and the supposed benefits of superfoods and vitamin infusions. Sadly, I witness individuals depriving themselves of vital nutrients while their cancer progresses.
While the fundamental message remains unchanged – avoid smoking, moderate alcohol intake, maintain a healthy diet, and stay active – it’s evident that relying solely on education and individual behavior isn’t sufficient. Recommendations from a recent UK analysis advocate for comprehensive social policies, including regulation and taxation, to shape public health and yield widespread benefits.
Empower Young Advocates
Navigating cancer diagnoses can be challenging for patients of all ages. From a 95-year-old undergoing surgery for breast cancer to a 40-year-old initially attributing weight loss to stress until diagnosed with advanced bowel cancer, both overdiagnosis and underdiagnosis pose significant challenges.
General practitioners (GPs) face the delicate task of balancing between conducting necessary tests and avoiding overwhelming the healthcare system. Primary care often grapples with time constraints, lack of continuity, and occasional lack of awareness. There’s a growing emphasis on educating GPs about cancer in younger individuals, but patients must also advocate for themselves, recognizing that persistent symptoms warrant attention regardless of age.
Improve Healthcare Systems
Negotiating the public hospital outpatient system can be akin to navigating a labyrinth, underscoring the challenges faced by doctors within it. Recent legal rulings have shed light on systemic shortcomings, highlighting the need for better processes.
While Australian public hospitals offer excellent cancer care, the journey from tests to specialist appointments can be fraught with delays, leading patients to self-fund various procedures. Urgent cases sometimes struggle to receive timely attention, despite the gravity of their conditions.
Improving healthcare systems isn’t solely about allocating more funds; it entails designing streamlined processes with input from frontline clinicians. Given the significant economic and emotional toll of cancer, it’s imperative to scrutinize every aspect of care delivery to best support patients.
